To kill a superbug
Scientists are recruiting phages, bacteria’s natural predators, as the antibiotic resistance crisis worsens.
Allison Parshall • November 19, 2021
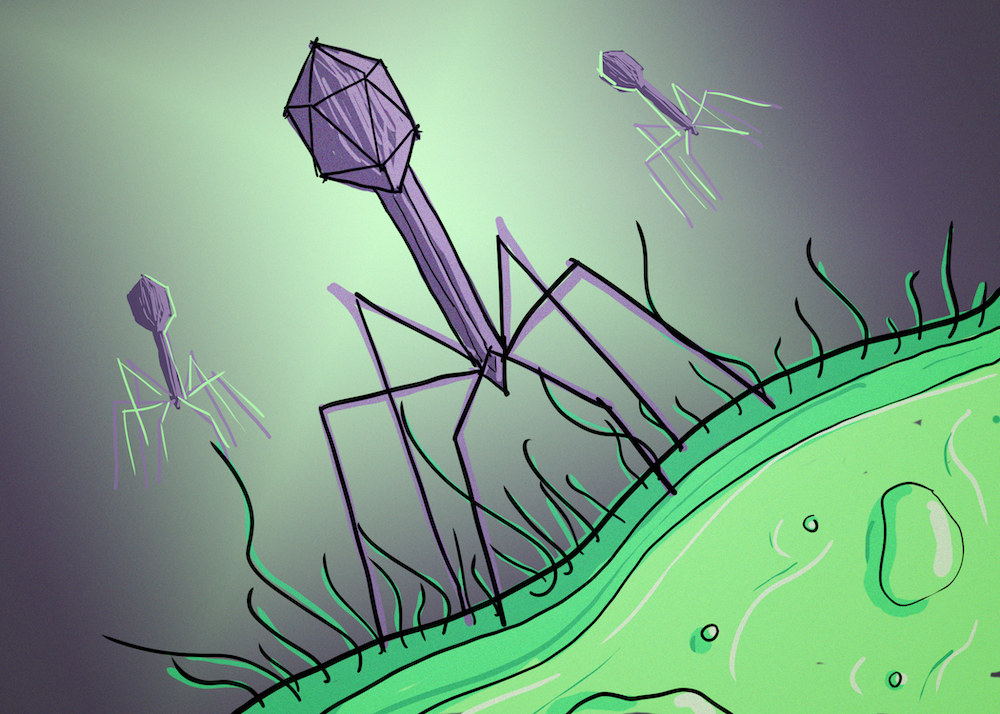
Phages are the most abundant biological entities on the planet, with countless varieties that infect specific types of bacteria. [Credit: Allison Parshall]
Ella Balasa was 26 when the antibiotics that kept her lungs from shutting down stopped working.
Balasa has cystic fibrosis, a genetic condition that leads to serious lung infections. For years, she cycled through the same drugs to fight them, but as the bacteria in her lungs evolved ways to fight back, the drugs became less and less effective.
Like nearly three million Americans every year, Balasa had an antibiotic-resistant infection complicated, in her case, by her underlying disease. By late 2018, she had run out of drug options. Her lungs were failing.
Desperate, Balasa turned to phage therapy, a century-old treatment being revived to fight so-called “superbugs” that have evolved resistance to antibiotic medicines and now kill 700,000 people each year — projected to hit 10 million per year by 2050. For now, phage therapy is available in the U.S. only on an emergency, case-by-case basis or through ongoing clinical trials. One such clinical trial — led by Balasa’s doctors — began this past March at Yale University, where the researchers have demonstrated a technique for pressuring a population of stubborn bacteria to give up their antibiotic resistance. The technique, called ‘phage steering’, is an alternate approach to traditional phage therapy that deploys complementary phages and antibiotics to combat resistant bacteria.
The concept of phage therapy is simple: turn bacteria’s natural predators against them. Phages are a category of viruses that infect only bacteria, not human cells. Since certain phages target specific types of bacteria, treating a bacterial infection becomes a matter of finding the right phage for the job. In practice, though, this simple concept can be costly and complicated. Researchers must scour water sources — often taking sewage samples — to find the right phage. Then they put the phage to the test through multiple trials in the lab against a sample of the patient’s bacteria.
Antibiotics are a much simpler and less expensive option, and their rise to prominence in the mid 20th century caused phage therapy — first used in 1919 — to fall into obscurity in the U.S. Now, as these overused drugs increasingly fail, interest has shifted back to the phages.
Over the last 20 years, around 2,000 instances of emergency phage treatment have been published across the world. The resulting reports have been promising, with success rates ranging from 40% to 100%, but they provide an incomplete picture of the safety and effectiveness of phage therapy. Until better data become available from clinical trials, the Food and Drug Administration likely will not approve phage therapy for widespread use in the U.S.
Balasa reached out to the Yale team in late 2018, when she was so sick she could barely travel. She nonetheless made the trip from Virginia to Connecticut to inhale a phage chosen specifically for her infection. “And lo and behold,” she recalls, “the infection cleared.”
In Balasa’s case, the phages were not solely responsible for this victory. Her doctors say that the antibiotics, previously all but useless, likely dealt the final blow. The bacteria in Balasa’s lungs were caught in a precise evolutionary trap, explains James Gurney, a biologist at the Georgia Institute of Technology who worked with Balasa’s doctors to analyze her case. The chosen phage targeted a part of the bacteria that protects against antibiotics, forcing them to give up their resistance to survive. The antibiotic medications she was taking were then able to finish the job.
This phenomenon is part of what Gurney calls “phage steering,” also known as “phage-antibiotic synergy.” Leveraging it requires detailed knowledge and careful testing of the phage, bacteria and antibiotics involved, and ultimately allows scientists to exploit the weak points of resistant bacteria — with the help of antibiotic treatments that the patient is likely already receiving.
Previous research has successfully used similar phage steering strategies for tackling different types of antibiotic-resistant bacteria, like E. coli, but it is still an uncommon technique. Far more common is the cocktail approach, Gurney explains, where many different types of phages come at the bacteria from many angles — sometimes with no antibiotics necessary for the final kill. Both techniques aim to prevent any bacteria from surviving and developing resistance to the phage.
The precision required for phage steering comes with many challenges. Jonathan Dennis of the University of Alberta stresses how lucky Balasa’s doctors were to find a phage that could pressure the bacteria into giving up its antibiotic resistance, as hitting that right on the head is very rare. For this reason, he is skeptical that phage steering will ever be successfully, broadly applied. Dennis doubts the technique could be used on most other bacteria, especially the complex species that he studies.
But Gurney is not alone in viewing phage steering as a way forward. For some, the precision of the technique is even a plus. “I think the medicines of the future are going to anticipate how the disease actually evolves with time,” predicts Anthony Maresso of the Baylor College of Medicine, who was not involved in Balasa’s treatment. He imagines a world of hyper-personalized and responsive infection treatment powered by phages. His lab compiles phages to treat resistant infections and can change the properties of a phage using a machine they call the “mutator.” The technique of engineering phages to target a particular patient’s infection is in its infancy, Maresso says, “but the science is telling us this is a possibility.”
Balasa, now 29, currently works as a professional patient advocate and consultant. She’s an avid proponent of the phage treatment she says saved her life, while also stressing the need for new antibiotics as our first line of defense.
Georgia Tech’s Gurney agrees that a multipronged approach is essential. “We had a ‘magical’ solution to this — the antibiotics,” he says. And by overusing them, “we screwed that up, quite frankly.”
“The magic bullets are finished,” he says. “We’ve got to use everything else now.”